**Mental Health: A Basic Human Right and the Barriers to Access**
Mental health is a basic human right for all people, according to the World Health Organization (WHO). Everyone, regardless of where they live or who they are, has the right to standard mental health care. However, unequal access to mental health services remains a significant challenge worldwide. This disparity is attributed not only to stigma but also to geographical location and neglect.
In theory, every person has the right to mental healthcare, but in practice, many cannot even afford the bus fare to visit a psychiatrist, let alone cover other associated expenses. Numerous barriers prevent access to mental healthcare services, including stigma, fear of judgment, and embarrassment. Alongside these social barriers, the cost of treatment is a major hurdle. When someone is advised to see a psychiatrist, many may nod in agreement, but far fewer follow through. This gap highlights that the underlying issues often go deeper than stigma and ignorance. Financial constraints, though frequently unspoken, are a very real and significant factor.
—
### Global Disparities in Mental Health Services
In the United States, only 47 percent of individuals with mental health needs received services in 2021. A shortage of mental health professionals exacerbates this problem, especially in rural states where psychiatrists are often unavailable. Furthermore, specialists such as child and adolescent psychiatrists and geriatric psychiatrists are scarce.
In countries like Bangladesh, Nigeria, and Kenya, the shortage is even more pronounced, with fewer than one mental health professional per 100,000 people. According to the World Health Organization’s Mental Health Atlas 2020, there are roughly 800 psychiatric units in general hospitals globally, with an average of only 2.1 beds per 100,000 population.
Outpatient psychiatric facilities exist, but only 1 percent offer dedicated child and adolescent mental health services. Additionally, 51 percent of psychiatrists work in urban private facilities, concentrating care in cities and neglecting rural populations. Approximately 45 percent work in the public sector, serving larger, often underserved populations.
—
### The Situation in Pakistan
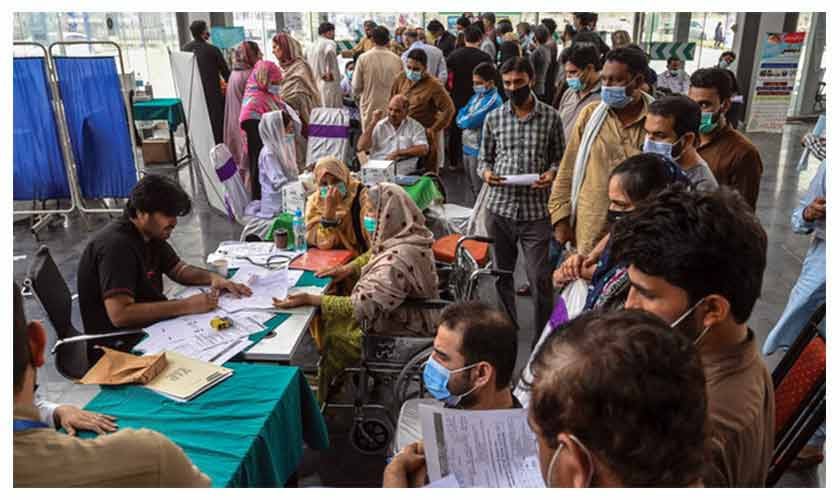
Pakistan faces similar challenges. Currently, there are only 900 psychiatrists serving a population of 255 million, resulting in limited access to care. Psychiatric services are concentrated in major cities, which means a single mental health facility often caters not only to urban populations but also to vast rural and peri-urban areas. This creates immense strain on resources and accessibility.
Private mental health services are largely unaffordable for most of the population in this low-middle-income country, further limiting access to care.
—
### Hidden Costs: The Invisible Burden
Financial burden remains a critical, often overlooked barrier to seeking mental health care. A study published in 2025 revealed that many patients with mental illness avoid seeking help due to the financial strain.
For patients in rural areas, transport fares, lost wages, and long waiting times at hospitals add to the burden before even receiving treatment. These hidden costs are rarely documented but weigh heavily on families already struggling to cope. Many travel long distances to reach mental health facilities, only to face crowded outpatient departments. In public hospitals, it is common for 300–400 patients to visit daily, with a single psychiatrist seeing up to 50 patients per day. This workload compromises the quality of care provided.
For rural patients, the intersection of financial stress and mental health issues intensifies their distress. Even when patients manage to seek help, the availability and affordability of medication are ongoing challenges, leading some to discontinue treatment due to cost.
A survey showed that among those who accessed mental healthcare in the past year, about 12 percent spent more than 20 percent of their family income on treatment.
—
### The Human Cost
What happens when mental healthcare is unaffordable?
– Depression deepens
– Anxiety worsens
– Daily functioning is impaired
– Families bear the emotional and financial burden
This cycle negatively affects individuals and their families, costing billions in lost productivity worldwide. In Pakistan, the impact adds to existing cycles of poverty and despair.
—
### Innovation and Hope
Despite these challenges, there is hope through innovative community-based programs. For example:
– **The Thinking Healthy Programme in Pakistan** focuses on improving maternal and child health.
– The **WHO Parents Skills Training Programme** has trained volunteers in rural Pakistan to identify and address developmental disorders.
– Mental health awareness campaigns via radio, television, and social media are helping to reduce stigma.
– During the COVID-19 pandemic, Pakistan held its first mental health coalition, bringing together organizations to formulate strategic plans and national advocacy.
– The Ministry of Planning, Development and Special Initiatives launched a digitalized mental health programme to strengthen intersectoral collaboration and close service gaps.
—
### What Must Change?
To improve access to mental healthcare, several steps are critical:
– **Increase the number of mental health facilities**, especially in underserved areas.
– Expand **postgraduate training centers** to produce more mental health professionals.
– Strengthen **rural healthcare systems** and integrate mental health services within them.
– Expand **tele-mental health facilities** to provide low-cost services in remote locations.
– Scale up **community-based models** like the Thinking Healthy Programme.
– Integrate **counselling into primary healthcare**.
– Promote mental health care that is **affordable, decentralized, and accessible**.
—
### Conclusion
Access to mental health care is not just about acceptance or awareness; affordability plays a crucial role. If care is not affordable, many individuals in need will remain silent, untreated, and unsupported.
Mental health is a fundamental human right and should be accessible to all. This requires compassionate, well-funded public policies that prioritize equitable mental health services for every community.
—
*Mental health is a human right—let us work together to make it a reality for everyone.*
https://www.thenews.com.pk/tns/detail/1350041-affording-care